20 mg/4 ml, 100 mg/20 ml
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
LABESOL (Labetalol Hydrochloride) is an adrenergic receptor blocking agent that has both selective alpha1-adrenergic and nonselective beta-adrenergic receptor blocking actions in a single substance. Labetalol (HCl) is a racemate. Chemically, Labetalol Hydrochloride is designated as 5-[1-hydroxy-2-(1-methyl-3-phenylpropyl)amino]ethyl]-salicylamide monohydrochloride. Its molecular formula is C19H24N2O3•HCl and its molecular weight is 364.87.
STRUCTURAL FORMULA :
Its structural formula is :
-Structure.jpg)
LABESOL is a clear, colourless to light yellow aqueous sterile isotonic solution for Intravenous Injection.
COMPOSITION :
Each ml contains :
Labetalol HCl USP 5 mg
Water for Injection USP q.s.
ACTIONS :
Labetalol combines both selective, competitive, alpha1-adrenergic blocking and nonselective, competitive, beta-adrenergic blocking activity in a single substance. Labetalol lowers blood pressure by blocking peripheral arteriolar α-adrenoceptors, thus reducing peripheral resistance and by concurrent β-blockade, protects the heart from reflex sympathetic drive that would otherwise occur. Cardiac output is not significantly reduced at rest or after moderate exercise. Increases in systolic blood pressure during exercise are reduced but corresponding changes in diastolic pressure are essentially normal. All these effects would be expected to benefit hypertensive patients. Labetalol does not adversely affect renal function and is particularly suitable for use in hypertensive patients with renal disease.
PHARMACODYNAMICS :
The capacity of Labetalol to block alpha receptors in man has been demonstrated by attenuation of the pressor effect of phenylephrine and by a significant reduction of the pressor response caused by immersing the hand in ice-cold water (“coldpressor test”). Labetalol’s beta1-receptor blockade in man was demonstrated by a small decrease in the resting heart rate, attenuation of tachycardia produced by Isoproterenol or exercise and by attenuation of the reflex tachycardia to the hypotension produced by amylnitrite. Beta2-receptor blockade was demonstrated by inhibition of the Isoproterenol induced fall in diastolic blood pressure. Both the alpha-and beta-blocking actions of orally administered Labetalol HCl contribute to a decrease in blood pressure in hypertensive patients. Labetalol consistently, in dose-related fashion, blunted increases in exercise induced blood pressure and heart rate and in their double product. The pulmonary circulation during exercise was not affected by Labetalol HCl dosing. Single oral doses of Labetalol HCl administered to patients with coronary artery disease had no significant effect on sinus rate, intraventricular conduction, or QRS duration. The atrioventricular (A-V) conduction time was modestly prolonged in two of seven patients. In another study, intravenous Labetalol slightly prolonged A-V nodal conduction time and atrial effective refractory period with only small changes in heart rate. The effects on A-V nodal refractoriness were inconsistent.
Labetalol produces dose-related falls in blood pressure without reflex tachycardia and without significant reduction in heart rate, presumably through a mixture of its alpha blocking and beta-blocking effects. Haemodynamic effects are variable, with small, nonsignificant changes in cardiac output seen in some studies but not others and small decreases in total peripheral resistance. Elevated plasma renins are reduced. Doses of Labetalol HCl that controlled hypertension did not affect renal function in mildly to severely hypertensive patients with normal renal function. Due to the alpha1-receptor blocking activity of Labetalol, blood pressure is lowered more in the standing than in the supine position and symptoms of postural hypotension can occur. During dosing with intravenous Labetalol HCl, the contribution of the postural component should be considered when positioning patients for treatment and patients should not be allowed to move to an erect position unmonitored until their ability to do so is established.
PHARMACOKINETICS :
Following intravenous infusion of Labetalol, the elimination half-life is about 5.5 hours and the total body clearance is approximately 33 ml/min/kg. The plasma half-life of Labetalol following oral administration is about 6 to 8 hours. In patients with decreased hepatic or renal function, the elimination half-life of Labetalol is not altered; however, the relative bioavailability in hepatically impaired patients is increased due to decreased “first-pass” metabolism. The metabolism of Labetalol is mainly through conjugation to glucuronide metabolites. These metabolites are present in plasma and are excreted in the urine and, via the bile, into the faeces. Approximately 55 % to 60 % of a dose appears in the urine as conjugates or unchanged labetalol within the first 24 hours of dosing. Labetalol has been shown to cross the placental barrier in humans. Only negligible amounts of the drug crossed the blood-brain barrier in animal studies. Labetalol is approximately 50 % protein bound. Neither haemodialysis nor peritoneal dialysis removes a significant amount of Labetalol from the general circulation (< 1 %).
INDICATIONS :
Severe hypertension when rapid control of blood pressure is essential. Anaesthesia when a hypotensive technique is indicated. Hypertensive episodes following acute myocardial infarction.
LABESOL is intended for intravenous use in hospitalized patients. DOSAGE MUST BE INDIVIDUALIZED depending upon the severity of hypertension and the response of the patient during dosing.
Patients should always be kept in a supine position during the period of intravenous drug administration. A substantial fall in blood pressure on standing should be expected in these patients. The patient’s ability to tolerate an upright position should be established before permitting any ambulation, such as using toilet facilities.
Either of two methods of administration of LABESOL may be used :
a) Repeated intravenous injection, or
b) Slow continuous infusion.
Repeated Intravenous Injection :
Initially, LABESOL should be given in 20 mg dose (which corresponds to 0.25 mg/kg for an 80 kg patient) by slow intravenous injection over a 2 minute period. Immediately before the injection and at 5 and 10 minutes after injection, supine blood pressure should be measured to evaluate response. Additional injections of 40 or 80 mg can be given at 10 minute intervals until a desired supine blood pressure is achieved or a total of 300 mg of LABESOL has been injected. The maximum effect usually occurs within 5 minutes of each injection and the duration of action is usually about 6 hours but may be as long as 18 hours.
Slow Continuous Infusion :
LABESOL is prepared for continuous intravenous infusion by diluting the vial contents with commonly used intravenous fluids (see below). Examples of two methods of preparing the infusion solution are : The contents of two 20 ml Vials (40 ml), are added to 160 ml of a commonly used intravenous fluid such that the resultant 200 ml of solution contains 200 mg of Labetalol HCl, 1 mg/ml. The diluted solution should be administered at a rate of 2 ml/min to deliver 2 mg/min. Alternatively, the contents of two 20 ml Vials (40 ml), of LABESOL are added to 250 ml of a commonly used intravenous fluid. The resultant 290 ml solution will contain 200 mg of Labetalol HCl, approximately 2 mg/3 ml. The diluted solution should be administered at a rate of 3 ml/min to deliver approximately 2 mg/min. The rate of infusion of the diluted solution may be adjusted according to the blood pressure response, at the discretion of the physician. To facilitate a desired rate of infusion, the diluted solution can be infused using a controlled administration mechanism, e.g. graduated burette or mechanically driven infusion pump. Since the half-life of Labetalol is 5 to 8 hours, steady-state blood levels (in the face of a constant rate of infusion) would not be reached during the usual infusion time period. The infusion should be continued until a satisfactory response is obtained and should then be stopped and oral Labetalol HCl started (see below). The effective intravenous dose is usually in the range of 50 to 200 mg. A total dose of up to 300 mg may be required in some patients.
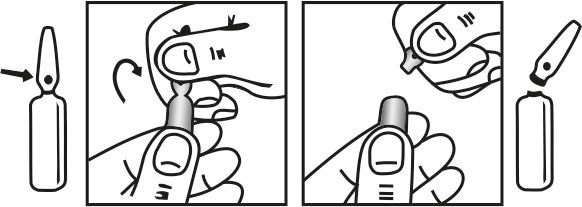
INSTRUCTION FOR USE OF AMPOULE (4 ml) :
The ampoule used in this product is equipped with O.P.C (One Point Cut) opening system. No ampoule file is needed to open the ampoule. The neck of the ampoule is prescored at the point of constriction. A coloured dot on the ampoule head helps to orientate the ampoule. Take the ampoule and face the coloured dot. Let the solution at the head of the ampoule to flow down by shaking or a gentle stroke. The ampoule opens easily by placing the thumb on the coloured dot and gently pressing downwards as shown.
DOSAGE :
Hypertension in pregnancy-Infusion should be started at 20 mg/hour, then doubled every 30 minutes until a satisfactory response is obtained or a dosage of 160 mg/hour is reached. Occasionally higher doses may be necessary. Hypertensive episodes following acute myocardial infarction-Infusion should be started at 15 mg/hour and gradually increased to a maximum of 120 mg/hour depending on the control of blood pressure. Hypertension due to other causes-Infuse at a rate of about 2 mg/min until a satisfactory response is obtained, then stop infusion. The effective dose is usually 50 - 200 mg but larger doses may be needed, especially in patients with phaeochromocytoma. The rate of infusion may be adjusted according to the response at the discretion of the physician. It is desirable to monitor the blood pressure and heart rate after injection and during infusion. In most patients, there is a small decrease in the heart rate; severe bradycardia is unusual but may be controlled by injecting atropine 1 - 2 mg intravenously. Respiratory function should be observed particularly in patients with any known impairment. LABESOL has been administered to patients with uncontrolled hypertension already receiving other hypotensive agents, including β-blocking drugs, without adverse effects. Hypotensive anaesthesia-induction should be with standard agents (e.g. sodium thiopentone) and anaesthesia maintained with nitrous oxide and oxygen with or without halothane. The recommended starting dose of LABESOL is 10 - 20 mg intravenously depending on the age and condition of the patient. Patients for whom halothane is contraindicated usually require a higher initial dose of LABESOL (25 - 30 mg). If satisfactory hypotension is not achieved after 5 minutes, increments of 5 - 10 mg should be given until the desired level of blood pressure is attained.
Blood Pressure Monitoring :
The blood pressure should be monitored during and after completion of the infusion or intravenous injection. Rapid or excessive falls in either systolic or diastolic blood pressure during intravenous treatment should be avoided. In patients with excessive systolic hypertension, the decrease in systolic pressure should be used as an indicator of effectiveness in addition to the response of the diastolic pressure.
Initiation of Dosing with Labetalol HCl Tablets :
Subsequent oral dosing with Labetalol HCl Tablets should begin when it has been established that the supine diastolic blood pressure has begun to rise. The recommended initial dose is 200 mg, followed in 6 to 12 hours by an additional dose of 200 or 400 mg, depending on the blood pressure response. Thereafter, inpatient titration with Labetalol HCl Tablets may proceed as follows :
Inpatients Titration instruction.
| Regimen | Daily Dose |
| 200 mg b.i.d. | 400 mg |
| 400 mg b.i.d. | 800 mg |
| 800 mg b.i.d. | 1,600 mg |
| 1200 mg b.i.d. | 2,400 mg |
* If needed, the total daily dose may be given in 3 divided dose.
The dosage of Labetalol HCl Tablets used in the hospital may be increased at 1-day intervals to achieve the desired blood pressure reduction.
Children :
Safety and efficacy in children have not been established.
CONTRAINDICATIONS :
LABESOL is contraindicated in 2nd or 3rd degree heart block, cardiogenic shock and other conditions associated with severe and prolonged hypotension or severe bradycardia. When peripheral vasoconstriction suggests low cardiac output, the use of LABESOL to control hypertensive episodes following acute myocardial infarction is contraindicated. Beta-blockers, even those with apparent cardioselectivity, should not be used in patients with asthma or a history of obstructive airways disease. Labetalol is contraindicated for patients known to have hypersensitivity to the medicine.
Hepatic Injury :
Severe hepatocellular injury, confirmed by rechallenge in at least one case, occurs rarely with Labetalol therapy. The hepatic injury is usually reversible, but hepatic necrosis and death have been reported. Injury has occurred after both short-and long-term treatment and may be slowly progressive despite minimal symptomatology. Similar hepatic events have been reported with a related research compound, Dilevalol HCl, including two deaths. Dilevalol HCl is one of the four isomers of Labetalol HCl. Thus, for patients taking Labetalol, periodic determination of suitable hepatic laboratory tests would be appropriate. Laboratory testing should be done at the very first symptom or sign of liver dysfunction (e.g. pruritus, dark urine, persistent anorexia, jaundice, right upper quadrant tenderness, or unexplained “flu-like” symptoms). If the patient has laboratory evidence of liver injury or jaundice, Labetalol should be stopped and not restarted.
Cardiac Failure :
Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure. Beta-blockade carries a potential hazard of further depressing myocardial contractility and precipitating more severe failure. Although betablockers should be avoided in overt congestive heart failure, if necessary, Labetalol can be used with caution in patients with a history of heart failure who are well compensated. Congestive heart failure has been observed in patients receiving Labetalol HCl. Labetalol does not abolish the inotropic action of digitalis on heart muscle.
In Patients Without a History of Cardiac Failure :
In patients with latent cardiac insufficiency, continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, patients should be fully digitalized and/or be given a diureticand the response should be observed closely. If cardiac failure continues despite adequate digitalization and diuretic, Labetalol therapy should be withdrawn (gradually, if possible).
Ischemic Heart Disease :
Angina pectoris has not been reported upon Labetalol discontinuation. However, following abrupt cessation of therapy with some beta-blocking agents in patients with coronary artery disease, exacerbations of angina pectoris and, in some cases, myocardial infarction have been reported. Therefore, such patients should be cautioned against interruption of therapy without the physician’s advice. Even in the absence of overt angina pectoris, when discontinuation of Labetalol is planned, the patient should be carefully observed and should be advised to limit physical activity. If angina markedly worsens or acute coronary insufficiency develops, Labetalol administration should be reinstituted promptly, at least temporarily and other measures appropriate for the management of unstable angina should be taken.
Nonallergic Bronchospasm (e.g. Chronic Bronchitis and Emphysema) :
Since Labetalol HCl at the usual intravenous therapeutic doses has not been studied in patients with non-allergic bronchospastic disease, it should not be used in such patients.
Pheochromocytoma :
Intravenous Labetalol has been shown to be effective in lowering blood pressure and relieving symptoms in patients with pheochromocytoma; higher than usual doses may be required. However, paradoxical hypertensive responses have been reported in a few patients with this tumor; therefore, use caution when administering Labetalol to patients with pheochromocytoma.
Diabetes Mellitus and Hypoglycemia :
Beta-adrenergic blockage may prevent the appearance of premonitory signs and symptoms (e.g. tachycardia) of acute hypoglycemia. This is especially important with labile diabetics. Beta-blockade also reduces the release of insulin in response to hyperglycemia; it may therefore be necessary to adjust the dose of antidiabetic drugs.
Major Surgery :
The necessity or desirability of withdrawing beta-blocking therapy before major surgery is controversial. Protracted severe hypotension and difficulty in restarting or maintaining a heartbeat have been reported with beta-blockers. The effect of Labetalol’s alpha-adrenergic activity has not been evaluated in this setting. A synergism between Labetalol and halothane anaesthesia has been shown.
Rapid Decreases of Blood Pressure :
Caution must be observed when reducing severely elevated blood pressure. A number of adverse reactions, including cerebral infarction, optic nerve infarction, angina and ischemic changes in the electrocardiogram, have been reported with other agents when severely elevated blood pressure was reduced over time courses of several hours to as long as 1 or 2 days. The desired blood pressure lowering should therefore be achieved over as long a period of time as is compatible with the patient’s status.
Risk of Anaphylactic Reaction :
While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Pregnancy : Pregnancy Category C.
Although no teratogenic effects have been demonstrated in animals, LABESOL should only be used during the first trimester of pregnancy if the potential benefit outweighs the potential risk. In humans Labetalol crosses the placental barrier and the possibility of the consequences of α and β-adrenoceptor blockade in the foetus and neonate should be borne in mind. Perinatal and neonatal distress (bradycardia, hypotension, respiratory depression, hypoglycaemia, hypothermia) has been rarely reported. Sometimes these symptoms developed a day or two after birth. Response to supportive measures (e.g. intravenous fluids and glucose) is usually prompt but with severe pre-eclampsia, particularly after prolonged intravenous Labetalol, recovery may be slower. This may be related to diminished liver metabolism in premature babies. Intra-uterine and neonatal deaths have been reported but other medicines (e.g. vasodilators, respiratory depressants) and the effects of pre-eclampsia, intra-uterine growth retardation and prematurity were implicated. Such clinical experience warns against unduly prolonging high dose Labetalol and delaying delivery and against co-administration of hydralazine.
Nursing mothers :
Small amounts of Labetalol (approximately 0.004 % of the maternal dose) are excreted in human milk. Caution should be exercised when Labetalol HCl is administered to a nursing woman.
Paediatric Use :
Safety and effectiveness in paediatric patients have not been established.
INTERACTIONS :
Since Labetalol HCl may be administered to patients already being treated with other medications, including other antihypertensive agents, careful monitoring of these patients is necessary to detect and treat promptly any undesired effect from concomitant administration.In one survey, 2.3 % of patients taking Labetalol orally in combination with tricyclic antidepressants experienced tremor as compared to 0.7 % reported to occur with Labetalol alone. The contribution of each of the treatments to this adverse reaction is unknown, but the possibility of a drug interaction cannot be excluded.
Drug possessing beta-blocking properties can blunt the bronchodilator effect of beta receptor agonist drugs in patients with bronchospasm; therefore, doses greater than the normal antiasthmatic dose of beta-agonist bronchodilator drugs may be required. Cimetidine has been shown to increase the bioavailability of Labetalol administered orally. Since this could be explained either by enhanced absorption or by an alteration of hepatic metabolism of Labetalol, special care should be used in establishing the dose required for blood pressure control in such patients. Synergism has been shown between halothane anaesthesia and intravenously administered Labetalol. During controlled hypotensive anaesthesia using Labetalol in association with halothane, high concentrations (3 % or above) of halothane should not be used because the degree of hypotension will be increased and because of the possibility of a large reduction in cardiac output and an increase in central venous pressure. The anaesthesiologist should be informed when a patient is receiving Labetalol. Labetalol blunts the reflex tachycardia produced by nitroglycerin without preventing its hypotensive effect. If Labetalol is used with nitroglycerin in patients with angina pectoris, additional antihypertensive effects may occur. Care should be taken if Labetalol is used concomitantly with calcium antagonists of the verapamil type.
SIDE EFFECTS :
LABESOL is usually well tolerated. Most adverse effects have been mild and transient and, in controlled trials involving 92 patients, did not require Labetalol withdrawal. Symptomatic postural hypotension (incidence, 58 %) is likely to occur if patients are tilted or allowed to assume the upright position within 3 hours of receiving Labetalol HCl. Moderate hypotension occurred in 1 of 100 patients while supine. Increased sweating was noted in 4 of 100 patients and flushing occurred in 1 of 100 patients.
Immune system disorders :
Common : Hypersensitivity.
Hypersensitivity reactions reported include rash, pruritus, dyspnoea and very rarely, drug fever or angioedema.
Cardiac disorders :
Rare : Bradycardia.
Very rare : Heart Block.
Vascular disorders :
Common : # Postural hypotension.
Very rare : Exacerbation of the symptoms of Raynaud’s Syndrome. Pronounced postural hypotension may occur if patients are allowed to assume the upright position within 3 hours of receiving LABESOL.
Respiratory, thoracic and mediastinal disorders :
Common : # Nasal congestion.
Hepatobilary disorders :
Common : Raised liver function tests.
Very rare : Hepatitis, hepatocellular jaundice, cholestatic jaundice, Hepatic necrosis.
The signs and symptoms of hepatobilary disorders are usually reversible on withdrawal of the drug.
OVERDOSAGES AND TREATMENT OF OVERDOSAGES :
Overdosage with Labetalol HCl causes excessive hypotension that is posture sensitive and sometimes, excessive bradycardia. Patients should be placed supine and their legs raised if necessary to improve the blood supply to the brain. If overdosage with Labetalol HCl follows oral ingestion, gastric lavage or pharmacologically induced emesis (using syrup of Ipecac) may be useful for removal of the drug shortly after ingestion. The following additional measures should be employed if necessary : Excessive bradycardia-administer atropine or epinephrine. Cardiac failure-administer a digitalis glycoside and a diuretic. Dopamine or dobutamine may also be useful. Hypotension-administer vasopressors, e.g. norepinephrine. There is pharmacologic evidence that norepinephrine may be the drug of choice. Bronchospasm-administer epinephrine and/or an aerosolized beta 2-agonist. Seizures-administer diazepam. In severe beta-blocker overdose resulting in hypotension and/or bradycardia, glucagon has been shown to be effective when administered in large doses (5 to 10 mg rapidly over 30 seconds, followed by continuous infusion of 5 mg per hour that can be reduced as the patient improves). Neither haemodialysis nor peritoneal dialysis removes a significant amount of Labetalol from the general circulation (< 1 %).
PHARMACEUTICAL PRECAUTIONS :
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
STORAGE :
Store between 2°C to 30°C (36°F to 86°F),
protected from light. Do not Freeze.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
LABESOL is available in 1 Ampoule of 4 ml and 1 Vial of 20 ml.

 Cardiovascular
Cardiovascular