
25 mg/2.5 ml, 50 mg/5 ml
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
acurium (Atracurium Besylate) is an intermediate-duration, nondepolarizing, skeletal muscle relaxant. Chemically, 2-(2-Carboxyethyl)-1,2,3,4-tetrahydro-6,7-dimethoxy-2-methyl-1-veratrylisoquinolinium benzenesulfonate, pentamethylene ester. The molecular formula is C65H82N2O18S2 and molecular weight is 1243.48.
STRUCTURAL FORMULA :
Its structural formula is :
-Structure.jpg)
ACURIUM is a sterile, clear, colourless aqueous solution filled in amber ampoule of suitable size.
COMPOSITION :
Each ml contains :
Atracurium Besylate USP 10 mg
Water for Injection USP q.s.
Contains no preservatives.
ACTIONS :
Atracurium besylate is a non-depolarising muscle relaxant with medium duration of action. Atracurium besilate, interacts specifically with neurophysiological processes at the motor end-plate by competitively displacing acetylcholine from its receptor sites. As a result of end-plate occupation by atracurium besilate, further depolarisation is inhibited. Subsequently, skeletal muscles are paralysed since stimulation by motor nerves cannot be transmitted to the muscles. Through inhibition of acetylcholine degradation by means of cholinesterase inhibitors, e.g. neostigmine or edrophonium, an increase of acetylcholine concentration is achieved at all cholinergic synapses. The balance between atracurium besylate (antagonist) and acetylcholine (agonist) is shifted in favour of the latter. As a result, stimulation of the muscle can reoccur.
PHARMACOKINETICS :
On intravenous injection both atracurium besylate and cisatracurium besylate undergo spontaneous degradation via Hofmann elimination (a non-enzymatic breakdown process occurring at physiological pH and temperature) to produce laudanosine and other metabolites. There is also ester hydrolysis by non-specific plasma esterases. The metabolites have no neuromuscular blocking activity. About 80 % of atracurium besylate is bound to plasma proteins. Atracurium besylate and its metabolites cross the placenta in clinically
insignificant amounts. Excretion of atracurium and cisatracurium is in urine and bile, mostly as metabolites. The elimination half-life has been reported to be about 20 minutes for atracurium and 22 to 29 minutes for cisatracurium but laudanosine has an elimination half-life of about 3 to 6 hours.
INDICATIONS :
ACURIUM is indicated, as an adjunct to general anaesthesia, to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation.
Administration :
FOR INTRAVENOUS USE.
ACURIUM should be administered intravenously. DO NOT GIVE ACURIUM BY INTRAMUSCULAR ADMINISTRATION. Intramuscular administration of ACURIUM may result in tissue irritation and there are no clinical data to support this route of administration. To avoid distress to the patient, ACURIUM should not be administered before unconsciousness has been induced. ACURIUM should not be mixed in the same syringe, or administered simultaneously through the same needle, with alkaline solutions (e.g., barbiturate solutions). As with other neuromuscular blocking agents, the use of a peripheral nerve stimulator will permit the most advantageous use of ACURIUM, minimizing the possibility of overdosage or underdosage, and assist in the evaluation of recovery.
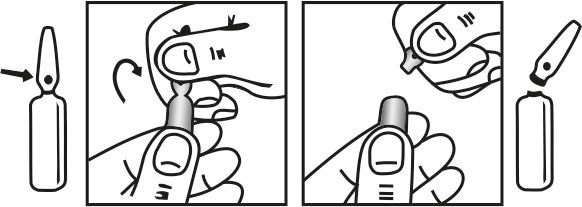
INSTRUCTION FOR USE OF AMPOULE :
The ampoule used in this product is equipped with O.P.C (One Point Cut) opening system. No ampoule file is needed to open the ampoule. The neck of the ampoule is prescored at the point of constriction. A coloured dot on the ampoule head helps to orientate the ampoule. Take the ampoule and face the coloured dot. Let the solution at the head of the ampoule to flow down by shaking or a gentle stroke. The ampoule opens easily by placing the thumb on the coloured dot and gently pressing downwards as shown.
Dosage :
Bolus Doses for Intubation and Maintenance of Neuromuscular Block Adults :
An ACURIUM dose of 0.4 to 0.5 mg/kg (1.7 to 2.2 times the ED95), given as an intravenous bolus injection, is the recommended initial dose for most patients. With this dose, good or excellent conditions for nonemergency intubation can be expected in 2 to 2.5 minutes in most patients, with maximum neuromuscular block achieved approximately 3 to 5 minutes after injection. Clinically required neuromuscular block generally lasts 20 to 35 minutes under balanced anaesthesia. Under balanced anaesthesia, recovery to 25 % of control is achieved approximately 35 to 45 minutes after injection, and recovery is usually 95 % complete approximately 60 minutes after injection.
ACURIUM is potentiated by isoflurane or enflurane anaesthesia. The same initial ACURIUM dose of 0.4 to 0.5 mg/kg may be used for intubation prior to administration of these inhalation agents; however, if ACURIUM is first administered under steady state of isoflurane or enflurane, the initial ACURIUM dose should be reduced by approximately one third, i.e., to 0.25 to 0.35 mg/kg, to adjust for the potentiating effects of these anaesthetic agents. With halothane, which has only a marginal (approximately 20 %) potentiating effect on ACURIUM, smaller dosage reductions may be considered. ACURIUM doses of 0.08 to 0.10 mg/kg are recommended for maintenance of neuromuscular block during prolonged surgical procedures. The first maintenance dose will generally be required 20 to 45 minutes after the initial ACURIUM, but the need for maintenance doses should be determined by clinical criteria. Because Atracurium Besylate lacks cumulative effects, maintenance doses may be administered at relatively regular intervals for each patient, ranging approximately from 15 to 25 minutes under balanced anaesthesia, slightly longer under isoflurane or enflurane. Higher ACURIUM doses (up to 0.2 mg/kg) permit maintenance dosing at longer intervals.
Paediatric Patients :
No ACURIUM dosage adjustments are required for paediatric patients 2 years of age or older. An ACURIUM dose of 0.3 to 0.4 mg/kg is recommended as the initial dose for infants (1 month to 2 years of age) under halothane anaesthesia. Maintenance doses may be required with slightly greater frequency in infants and children than in adults.
Special Considerations :
An initial ACURIUM dose of 0.3 to 0.4 mg/kg, given slowly or in divided doses over one minute, is recommended for adults, adolescents, children, or infants with significant cardiovascular disease and for adults, adolescents, children, or infants with any history (e.g., severe anaphylactoid reactions or asthma) suggesting a greater risk of histamine release. Dosage reductions must be considered also in patients with neuromuscular disease, severe electrolyte disorders, or carcinomatosis in which potentiation of neuromuscular block or difficulties with reversal have been demonstrated. There has been no clinical experience with Atracurium Besylate Injection in these patients, and no specific dosage adjustments can be recommended. No ACURIUM dosage adjustments are required for patients with renal disease. An initial ACURIUM dose of 0.3 to 0.4 mg/kg is recommended for adults following the use of succinylcholine for intubation under balanced anaesthesia. Further reductions may be desirable with the use of potent inhalation anaesthetics. The patient should be permitted to recover from the effects of succinylcholine prior to Atracurium Besylate Injection administration. Insufficient data are available for recommendation of a specific initial ACURIUM dose for administration following the use of succinylcholine in children and infants.
Infusion in the Intensive Care Unit (ICU) :
Multiple factors in anaesthesia practice are suspected of triggering malignant hyperthermia (MH), a potentially fatal hypermetabolic state of skeletal muscle. Halogenated anaesthetic agents and succinylcholine are recognized as the principal pharmacologic triggering agents in MH-susceptible patients; however, since MH can develop in the absence of established triggering agents, the clinician should be prepared to recognize and treat MH in any patient scheduled for general anaesthesia. Reports of MH have been rare in cases in which Atracurium Besylate has been used. In studies of MH-susceptible animals (swine) and in a clinical study of MH-susceptible patients, Atracurium Besylate did not trigger this syndrome. Resistance to nondepolarizing neuromuscular blocking agents may develop in burn patients. Increased doses of nondepolarizing muscle relaxants may be required in burn patients and are dependent on the time elapsed since the burn injury and the size of the burn. The safety of Atracurium Besylate has not been established in patients with bronchial asthma.
Little information is available on the plasma levels and clinical consequences of atracurium metabolites that may accumulate during days to weeks of atracurium administration in ICU patients. Laudanosine, a major biologically active metabolite of atracurium without neuromuscular blocking activity, produces transient hypotension and, in higher doses, cerebral excitatory effects (generalized muscle twitching and seizures) when administered to several species of animals. There have been rare spontaneous reports of seizures in ICU patients who have received atracurium or other agents. These patients usually had predisposing causes (such as head trauma, cerebral oedema, hypoxic encephalopathy, viral encephalitis, uraemia). There are insufficient data to determine whether or not laudanosine contributes to seizures in ICU patients.
WHENEVER THE USE OF ATRACURIUM BESYLATE OR ANY NEUROMUSCULAR BLOCKING AGENT IS CONTEMPLATED IN THE ICU, IT IS RECOMMENDED THAT NEUROMUSCULAR TRANSMISSION BE MONITORED CONTINUOUSLY DURING ADMINISTRATION WITH THE HELP OF A NERVE STIMULATOR. ADDITIONAL DOSES OF ATRACURIUM BESYLATE OR ANY OTHER NEUROMUSCULAR BLOCKING AGENT SHOULD NOT BE GIVEN BEFORE THERE IS A DEFINITE RESPONSE TO T1 OR TO THE FIRST TWITCH. IF NO RESPONSE IS ELICITED, INFUSION ADMINISTRATION SHOULD BE DISCONTINUED UNTIL A RESPONSE RETURNS.
Pregnancy : Category C
There are no adequate data on the use of atracurium besylate during pregnancy. Animal studies of effects on pregnancy, embryo/foetal development, parturition and post natal development are incomplete. Atracurium besylate should only be administered during pregnancy after careful risk-benefit assessment. Placental transfer is low. Applications within the recommended dose range in caesarean section patients showed no detrimental effects on the new-born. Therefore, atracurium besylate is also suitable for maintenance of muscle relaxation during caesarean section.
Use in obstetrics
It is not known whether muscle relaxants administered during vaginal delivery have immediate or delayed adverse effects on the foetus or increase the likelihood that resuscitation of the newborn infant will be necessary. The possibility that a forceps delivery will be necessary may increase. In an open study, atracurium besylate (0.3 mg/kg) was administered to 26 pregnant women during delivery by caesarean section. No harmful effects were attributable to atracurium in any of the newborn infants, although small amounts of atracurium were shown to cross the placental barrier. The possibility of respiratory depression in the newborn infant should always be considered following caesarean section during which a neuromuscular blocking agent has been administered. In patients receiving magnesium sulfate, the reversal of neuromuscular blockade may be unsatisfactory and the atracurium dose should be lowered as indicated.
Nursing mothers :
It is not known whether atracurium besylate passes into breast milk. Due to the short half-life, an influence on the infant is not to be expected if the mother starts breast-feeding (again) after the effects of the substance have worn off. As a precaution restart breast-feeding 24 hours after administration of atracurium besilate.
Paediatric Use :
Neonates up to 1 month of age may be more sensitive to the effects of nondepolarizing neuromuscular blocking agents
EFFECTS ON ABILITY TO DRIVE AND USE MACHINES :
As the medicinal product is administered under general anaesthesia, the patient must not drive, operate machinery or work in exposed situations after anaesthesia. The time factor should be decided individually by the physician. The patient should be accompanied on his way home and should not ingest alcohol.
INTERACTIONS AND INCOMPATIBILITIES :
As with other nondepolarising neuromuscular blocking agents, the magnitude and/or duration of atracurium’s effects may be increased as a result of an interaction with the following agents.
Inhalation anaesthetics :
Atracurium is potentiated by isoflurane and enflurane anaesthesia, and only marginally potentiated by halothane anaesthesia.
Antibiotics :
Including the aminoglycosides, polymyxins, spectinomycin, tetracyclines, lincomycin, clindamycin and vancomycin.
Antiarrhythmic drugs :
Lignocaine, procainamide, quinidine.
Beta-Blockers :
propranolol.
Calcium channel blockers :
Verapamil.
Diuretics :
Frusemide, thiazides, acetazolamide and possibly mannitol.
Ganglion blocking agents :
Trimetaphan, hexamethonium.
Others :
Magnesium sulphate, catamite, lithium salts, and quinine. It is not known whether the prior use of other nondepolarising neuromuscular blocking agents has any affect on the activity of atracurium. The prior use of suxamethonium reduces the onset (to maximum blockade) by approximately 2 to 3 minutes, and may increase the depth of neuromuscular blockade induced by atracurium. Therefore, atracurium should not be administered until the patient has recovered from suxamethonium induced neuromuscular blockade. If suxamethonium is used to prolong the neuromuscular blocking effects of atracurium, this may result in a prolonged and complex block which can be difficult to reverse with anticholinesterase drugs. If other muscle relaxants are used during the same procedure, the possibility of a synergistic or antagonistic effect should be considered.
Rarely, certain drugs may aggravate or unmask latent myasthenia gravis or actually induce a myasthenic syndrome. Such drugs include various antibiotics, beta-blockers (propranolol, oxprenolol), antiarrhythmic drugs (procainamide, quinidine), antirheumatic drugs (chloroquine, dpenicillamine), trimetaphan, chlorpromazine, steroids, phenytoin and lithium. In these situations a consequent increased sensitivity to atracurium would be expected. The onset of neuromuscular blockade is likely to be lengthened and the duration of blockade shortened in patients receiving chronic anticonvulsant therapy (e.g. carbamazepine, phenytoin).
Incompatibilities :
Alkaline solutions such as barbiturate injections should not be mixed in the same syringe, or administered simultaneously through the same intravenous needle, with atracurium. Alkaline solutions may change the pH of the acidic atracurium solution, resulting in inactivation of atracurium or precipitation of a free acid. Spontaneous degradation of atracurium has been shown to occur more rapidly when the medication is diluted with lactated Ringer’s injection than when the medication is diluted with 0.9 % sodium chloride injection. Therefore, it is recommended that lactated Ringer’s injection not be used to prepare intravenous infusion solutions containing atracurium.
SIDE EFFECTS :
Adverse reactions are listed below by system organ class and frequency. Frequencies are defined as : very common (≥ 1/10), common (≥ 1/100 and < 1/10), uncommon (≥ 1/1000 and < 1/100), rare (≥ 1/10,000 and < 1/1000), very rare (< 1/10,000). Very common, common and uncommon frequencies were determined from clinical trial data. Rare and very rare frequencies were generally derived from spontaneous data. The frequency classification “Not known” has been applied to those reactions where a frequency could not be estimated from the available data.
OVERDOSAGE :
The main signs of over-dose are prolonged muscle paralysis and its consequences.
TREATMENT OF OVERDOSAGE :
If cardiovascular support is necessary, this should include proper positioning of the patient, fluid administration/volume substitution, and the use of vasopressor agents if necessary. It is essential to maintain a patent airway together with assisted positive pressure ventilation until adequate spontaneous respiration reappears. Full sedation will be required since consciousness is not impaired. Recovery may be accelerated by the administration of anticholinesterase agents accompanied by atropine or glycopyrrolate, once evidence of spontaneous recovery is present.
PHARMACEUTICAL PRECAUTIONS :
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
STORAGE :
Store in a refrigerator between 2° to 8°C (36° to 46°F), protected from light.
Do not freeze.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
ACURIUM is supplied as below :
![]()
Disclaimer : For the use of a Registered Medical Practitioner or a Hospital or a Institution only. Also it is not intended to be used by healthcare professionals or patients for the purpose of prescribing or administering these products. Questions regarding the complete and current content of product labeling / specification / presentation should be directed to SGPharma.

 Cardiovascular
Cardiovascular





