50 mcg/ml, 100 mcg/ml
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
OCTOSTAT (Octreotide acetate) is a synthetic analogue of the naturally occurring hormone somatostatin with similar physiological action, but longer biological half-life and higher potency. Chemically, Octreotide acetate is L-Cysteinamide,D-phenylalanyl-L-Cysteinyl-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-[2-hydroxymethyl)propyl]-,cyclic(2→7)-disulfide, [R-(R*,R*)] acetate salt. Its molecular formula is C49H66N10O10S2 .C2H4O2 and its molecular weight is 1079.40. Its amino acid sequence is
-1.jpg)
STRUCTURAL FORMULA :
Its structural formula is :
-Structure.jpg)
OCTOSTAT is sterile, clear colourless solution filled in 1 ml amber O.P.C. ampoule.
COMPOSITION :
OCTOSTAT 50 mcg
Each ml contains :
Octreotide Acetate
equivalent to Octreotide 50 mcg
Water for Injections I.P. q.s.
Contains no preservatives.
OCTOSTAT 100 mcg
Each ml contains :
Octreotide Acetate
equivalent to Octreotide 100 mcg
Water for Injections I.P. q.s.
Contains no preservatives.
ACTIONS :
Octreotide is a synthetic octapeptide derivative of naturally occurring somatostatin with similar pharmacological effects, but with a longer duration of action. It inhibits pathologically increased secretion of growth hormone and of peptides and serotonin produced within the gastroenteropancreatic endocrine (GEP) system. In animals, octreotide is a more potent inhibitor of growth hormone, glucagon and insulin release than somatostatin with greater selectivity for growth hormone and glucagon suppression. In normal healthy subjects octreotide, like somatostatin has been shown to inhibit
• Release of growth hormone stimulated by arginine, exercise and insulin-induced hypoglycaemia.
• Postprandial release of insulin, glucagon, gastrin other peptides of the gastroenteropancreatic system; arginine-stimulated release of insulin and glucagons.
• Thyrotropin-releasing hormone (TRH) - stimulated release of thyroid stimulating hormone (TSH).
Unlike somatostatin, octreotide inhibits growth hormone preferentially over insulin and its administration is not followed by rebound hypersecretion of hormones (i.e. growth hormone in patients with acromegaly). For patients undergoing pancreatic surgery, the peri and post-operative administration of octreotide reduces the incidence of typical post-operative complications (e.g. pancreatic fistula, abscess and subsequent sepsis, post-operative acute pancreatitis). In patients with acromegaly, octreotide consistently lowers GH and normalises IGF-1 serum concentrations in the majority of patients. In most patients, octreotide markedly reduces the clinical symptoms of the disease, such as headache, perspiration, paresthesia, fatigue, osteoarthralgia and carpal tunnel syndrome. In individual patients with GH-secreting pituitary adenoma, octreotide was reported to lead to shrinkage of the tumour mass. For patients with functional tumours of the gastroenteropancreatic endocrine system, treatment with octreotide provides continuous control of symptoms related to the underlying disease. The effect of octreotide in different types of gastroenteropancreatic tumours are as follows :
Carcinoid tumours :
Administration of octreotide may result in improvement of symptoms, particularly of flushing and diarrhoea. In many cases, this is accompanied by a falling plasma serotonin and reduced urinary excretion of 5-hydroxyindole acetic acid.
VIPomas :
The biochemical characteristics of these tumours is overproduction of vasoactive intestinal peptide (VIP). In most cases, administration of octreotide results in alleviation of the severe secretory diarrhoea typical of the condition, with consequent improvement in quality of life. This is accompanied by an improvement in associated electrolyte abnormalities, e.g. hypokalaemia, enabling enteral and parenteral fluid and electrolyte supplementation to be withdrawn. Clinical improvement is usually accompanied by a reduction in plasma VIP levels, which may fall into the normal reference range.
Glucagonomas :
Administration of octreotide results in most cases in substantial improvement of the necrolytic migratory rash which is characteristic of the condition. The effect of octreotide on the state of mild diabetes mellitus which frequently occurs is not marked and, in general, does
not result in a reduction of requirements for insulin or oral hypoglycaemic agents. Octreotide produces improvement of diarrhoea, and hence weight gain, in those patients affected. Although administration of octreotide often leads to an immediate reduction in plasma glucagon levels, this decrease is generally not maintained over a prolonged period of administration, despite continued symptomatic improvement.
Acute variceal bleeding :
Although the exact mechanisms of acute haemodynamic changes are not known. Octreotide was observed to decrease the hepatic venous pressure gradient & the azygos blood flow with minimal effects on systemic haemodynamics.
PHARMACOKINETICS :
After subcutaneous injection, octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/ml (100 mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d (1500 mcg/day). In healthy volunteers the distribution of octreotide from plasma was rapid (tα½ = 0.2 h ), the volume of distribution (Vdss) was estimated to be 13.6 l & the total body clearance ranged from 7 l/hr to 10 l/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65 % was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin. The elimination of octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 - 3 minutes with the natural hormone. The duration of action of octreotide is variable but extends upto 12 hours depending upon the type of tumour. About 32 % of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46 %) and a significant decrease in the clearance (26 %) of the drug.
In patient with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/ml (100 mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 l and the total body clearance was increased to 18 l/hr. The mean percent of the drug bound was 41.2 %. The disposition and elimination half-lives were similar to normals. In patients with renal impairment the elimination of octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR 40-60 ml/min) octreotide t½ was 2.4 hours and total body clearance was 8.8 l/hr, in moderate impairment (ClCR10 - 39 ml/min) t½ was 3.0 hours and total body clearance 7.3 l/hr, and in severely renally impaired patients not requiring dialysis (ClCR < 10 ml/min) t½ was 3.1 hours and total body clearance was 7.6 l/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 l/hr to 4.5 l/hr). Patients with liver cirrhosis showed prolonged elimination of drug, with octreotide t½ increasing to 3.7 hr and total body clearance decreasing to 5.9 l/hr, whereas patients with fatty liver disease showed t½ increased to 3.4 hr and total body clearance of 8.2 l/hr.
INDICATIONS :
• OCTOSTAT are indicated for the relief of symptoms associated with neuroendocrine (particularly carcinoid) tumours and acromegaly.
• Octreotide is also licensed for the prevention of complications following pancreatic surgery.
• Octreotide may be valuable in reducing vomiting in palliative care (Octreotide, which stimulates water and electrolyte absorption and inhibits water secretion in the small bowel, can be used by subcutaneous infusion in a dose of 300 – 600 micrograms/24 hours to reduce intestinal secretions and vomiting) and in stopping variceal bleeding.
Administration :
OCTOSTAT may be administered subcutaneously or intravenously. Subcutaneous injection is the usual route of administration of OCTOSTAT for control of symptoms.
Subcutaneous administration :
Patients who are to self-administer the drug by s.c. injection must receive precise directions from the physician or the nurse. To reduce local discomfort, it is recommended that the solution should be at room temperature before injection. Multiple injections at short intervals at the same site should be avoided. Ampoules should be opened just prior to administration, and any unused portion discarded.
Intravenous infusion :
Parenteral drug products should be inspected visually for discolouration and particulate matter prior to administration. OCTOSTAT is physically and chemically stable for 24 hours in sterile physiological saline solutions or sterile solutions of dextrose (glucose) 5 % in water. However, because OCTOSTAT can affect glucose homeostasis, it is recommended that physiological saline solutions be used rather than dextrose. The diluted solutions are physically and chemically stable for at least 24 hours below 25° C. From a microbiological point of view, the diluted solution should preferably be used immediately. If the solution is not used immediately, storage prior to use is the responsibility of the user and should be at 2-8° C. Before administration the solution has to be brought to room temperature again.
The cumulated time between reconstitution, dilution with infusion media, storage in a refrigerator, and end of administration must not be longer than 24 hours. In cases where OCTOSTAT is to be administered by I.V. infusion, the contents of one 0.5 mg ampoule should normally be dissolved in 60 ml physiological saline, and the resulting solution should be infused by means of an infusion pump. This should be repeated as often as necessary until the prescribed duration of treatment is reached. OCTOSTAT has also been infused in lower concentrations. OCTOSTAT is not compatible in Total Parenteral Nutrition (TPN) solutions because of the formation of a glycosyl octreotide conjugate which may decrease the efficacy of the product.
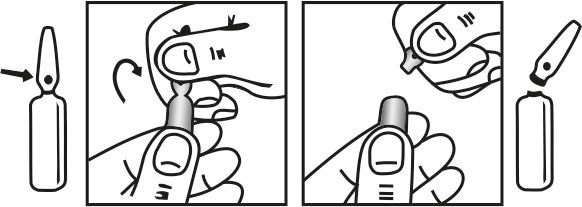
INSTRUCTION FOR USE OF AMPOULE :
The ampoule used in this product is equipped with O.P.C. (One Point Cut) opening system. No ampoule file is needed to open the ampoule. The neck of the ampoule is prescored at the point of constriction. A coloured dot on the ampoule head helps to orientate the ampoule. Take the ampoule and face the coloured dot. Let the solution at the head of the ampoule to flow down by shaking or a gentle stroke. The ampoule opens easily by placing the thumb on the coloured dot and gently pressing downwards as shown.
Dosage :
• Symptoms associated with carcinoid tumours with features of carcinoid syndrome, VIPomas, glucagonomas, by subcutaneous injection, initially 50 micrograms once or twice daily, gradually, increased according to response to 200 micrograms 3 times daily (higher doses required exceptionally); maintenance doses variable; in carcinoid tumours discontinue after 1 week if no effect; if rapid response required, initial dose by intravenous injection (with ECG monitoring and after dilution to a concentration of 10 – 50 % with sodium chloride 0.9 % injection).
• Acromegaly : short-term treatment before pituitary surgery or long-term treatment in those inadequately controlled by other treatment or until radiotherapy becomes fully effective by subcutaneous injection,100 – 200 micrograms 3 times daily; discontinue if no improvement within 3 months.
CONTRAINDICATIONS :
Hypersensitivity to the drug formulation or any of its components.
WARNINGS :
Single doses of octreotide acetate have been shown to inhibit gallbladder contractility and decrease bile secretion in normal volunteers. In clinical trials (primarily patients with acromegaly or psoriasis), the incidence of biliary tract abnormalities was 63 % (27 % gallstone, 24 % sluge without stones, 12 % biliary duct dilatation). The incidence of stone or sludge in patients who received octreotide acetate for 12 months or longer was 52 %. Less than 2 % of patient treated with octreotide acetate for 1 month or less developed gallstones. The incidence of gallstone did not appear related of age, sex or dose. Like patients without gallbladder abnormalities, the majority of patients developing gallbladder abnormalities on ultrasound had gastrointestinal symptoms. The symptoms were not specific for gallbladder disease. A few patients developed acute cholecystitis, ascending cholangitis, biliary abstraction, cholestatic hepatitis, or pancreatitis during octreotide acetate therapy or following its withdrawal.
PRECAUTIONS :
• Growth hormone-secreting pituitary tumours can expand causing serious complications; during treatment with somatostatin analogues patients should be monitored for signs of tumour expansion (e.g. visual field defects). Ultrasound examination of the gallbladder is recommended before treatment and at intervals of 6 – 12 months during treatment (avoid abrupt withdrawal of short-acting octreotide—see Side-effects). In insulinoma an increase in the depth and duration of hypoglycaemia may occur (observe patients when initiating treatment and changing doses); in diabetes mellitus, insulin or oral antidiabetic requirements may be reduced.
• Hepatic impairment, monitor thyroid function on long term therapy.
Pregnancy : Category B
Possible effect on foetal growth; caution should therefore be exercised by balancing the potential hazard.
Breast feeding :
It is not known whether OCTOSTAT is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in breast fed infants from OCTOSTAT, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of drug to the mother.
INTERACTIONS :
Antidiabetics : Octreotide possibly reduces requirements for insulin, metformin, repaglinide and sulfonyureas.
Ciclosporin : Octreotide reduces plasma concentration of ciclosporin.
Dopaminergics : Octreotide increases plasma concentration of bromocriptine.
Ulcer-healing drugs : Octreotide possibly delays absorption of cimetidine.
SIDE EFFECTS :
- Gastro-intestinal disturbances including anorexia, nausea, vomiting, abdominal pain and bloating, flatulence, diarrhoea, and steatorrhoea may occur. Postprandial glucose tolerance may be impaired and rarely persistent hyperglycaemia occurs with chronic administration; hypoglycaemia has also been reported.
- Gallstones have been reported after long-term treatment (abrupt withdrawal of subcutaneous octreotide is associated with biliary colic and pancreatitis). Pain and irritation may occur at the injection site and sites should be rotated. Rarely, pancreatitis has been reported shortly after administration.
- Rarely altered liver function tests, hepatitis and transient alopecia.
OVERDOSAGE :
Doses of upto 2000 mcg octreotide given as subcutaneous t.i.d for several months have been well tolerated. No life-threatening reactions have been reported after acute overdosage. The maximum single dose so far given to an adult so far has been 1 mg by intravenous bolus injection. The observed signs and symptoms were a brief drop in heart rate, facial flushing, abdominal cramps, diarrhoea, an empty feeling in the stomach and nausea, which resolved in 24 hours of drug administration.
TREATMENT OF OVERDOSAGE :
The management of overdosage is symptomatic.
PHARMACEUTICAL PRECAUTIONS :
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
STORAGE :
Store in a refrigerator between 2°C to 8°C (36° to 46°F), protected from light.
Do not freeze.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
-Table.jpg)
Disclaimer : For the use of a Registered Medical Practitioner or a Hospital or a Institution only. Also it is not intended to be used by healthcare professionals or patients for the purpose of prescribing or administering these products. Questions regarding the complete and current content of product labeling / specification / presentation should be directed to SGPharma.

 Cardiovascular
Cardiovascular








