100 mg, 200 mg
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
DACONE (Dacarbazine) is a cell-cycle non-specific antineoplastic that is thought to function as an alkylating agent after it has been activated in the liver. Chemically, Dacarbazine is 1 H -Imidazole-4-carboxamide, 5-(3,3-dimethyl-1-triazenyl)-. The molecular formula is C6H10N6O and molecular weight is 182.18.
STRUCTURAL FORMULA :
Its structural formula is :
-Structure.jpg)
DACONE is a white to pale yellow powder filled in a amber tubular vial of suitable size.
COMPOSITION :
DACONE – 100
(Lyophilised)
Each vial contains :
Dacarbazine USP 100 mg
(Excipients - Citric Acid USP, Mannitol USP)
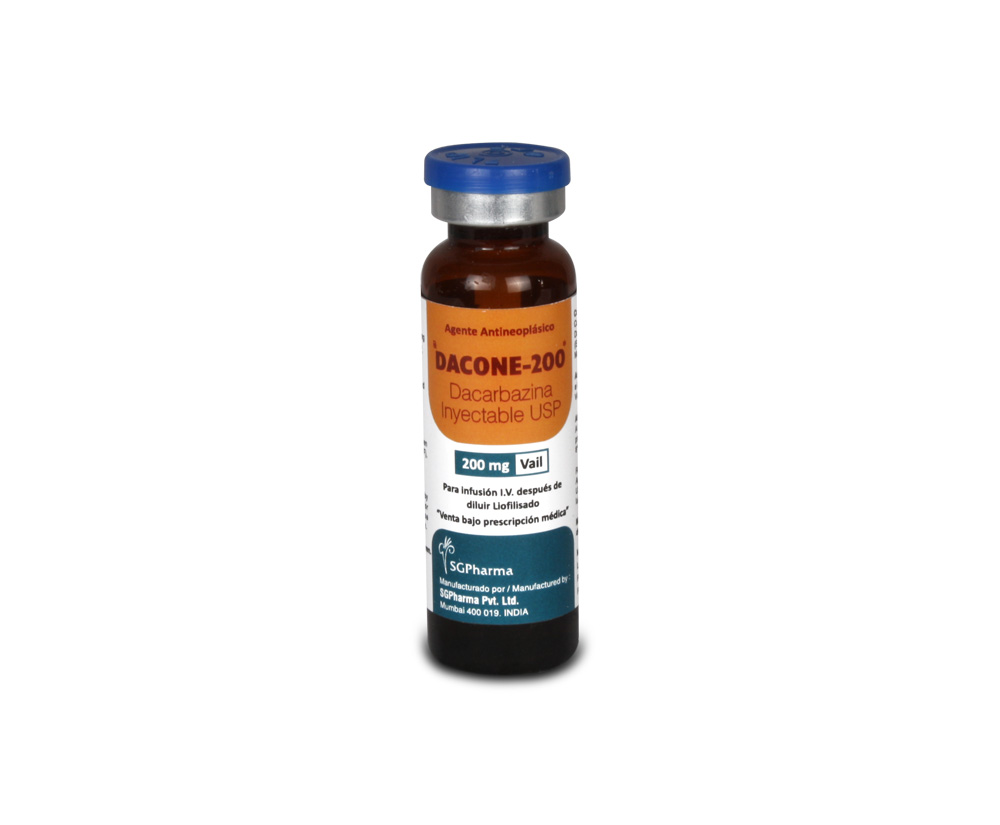
DACONE – 200
(Lyophilised)
Each vial contains :
Dacarbazine USP 200 mg
(Excipients - Citric Acid USP, Mannitol USP)
ACTIONS :
Relationship to other drugs : Dacarbazine is a structural analogue of 5-amino-imidazole-4-carboxamide which is an intermediate in purine biosynthesis.
Site and mode of action : This drug inhibits cell replication by an unknown mechanism. However, three possible mechanisms have been postulated :Since dacarbazine is an analogue of 5-amino-imidazole-4-carboxamide, an intermediate in the de novo biosynthesis of purine, it might interfere with purine biosynthesis and hence DNA bio-synthesis. This appears to be true at high concentrations of the drug, but low concentrations appear to enhance DNA, RNA and protein biosynthesis.One metabolite of dacarbazine, diazomethane, is an alkylating agent and may act in the same way as the nitrogen mustards. The drug might act as a sulphydryl reagent since the inhibition of bacterial growth by dacarbazine can be prevented by glutathione.
PHARMACOKINETICS :
Absorption : Dacarbazine is poorly and erratically absorbed from the gastrointestinal tract, which could result in unpredictable tumour responses and possible increased toxicity. Therefore the drug is recommended for intravenous administration only. Peak plasma concentrations of about 8 mcg/ml are reached immediately following administration of dacarbazine 4.5 mg/kg by intravenous push.
Distribution : Plasma protein binding is 5 %. Kinetics in plasma are biphasic; the initial (distribution) half-life is only 20 minutes, terminal half-life is 0.5 – 3.5 hours.
Metabolism / elimination : Dacarbazine is N-demethylated by liver microsomal enzymes to yield CO2 which is excreted in expired air and aminoimidazole-carboxamide (AIC) which is excreted in the urine. About half the drug remains unchanged and is rapidly excreted by tubular secretion. As dacarbazine is approximately 50 % metabolised by the liver and the remaining unchanged drug and metabolites are excreted in the urine, impairment of hepatic or renal function may require a reduction in dosage to avoid toxicity. Plasma concentrations of dacarbazine appear to decline in a biphasic manner. The initial phase half life (t½α) is very short, with one study reporting t½α as 2.9 minutes. The terminal phase half life (t½β) is consistently longer 41.4 to 75 minutes. In one patient with renal and hepatic dysfunction, the t½α was 55 minutes and the t½β was 7.2 hours.
INDICATIONS :
DACONE is used as a chemotherapeutic agent in metastatic malignant melanoma, sarcoma and Hodgkin’s disease. DACONE has also been shown to be of value in the treatment of other malignant diseases including carcinoma of the colon, ovary, breast, lung, testicular teratoma and solid tumours in children, when used in combination with other chemotherapeutic agents. Note : The use of dacarbazine is restricted to hospitals with an oncology service.
Administration :
Administration is by the intravenous route only. Dacarbazine 100 mg and 200 mg vials should be reconstituted with 9.9 ml and 19.7 ml respectively, of Water for Injections. The use of dacarbazine should be confined to physicians experienced in oncology or haematology respectively. The resulting solution is hypotonic and will contain 10 mg/ml of dacarbazine with a pH of 3 to 4. Intravenous injection may be given over about one minute. Extravasation of the drug into surrounding tissue during intravenous administration may result in tissue damage and severe pain. Dacarbazine is sensitive to light exposure. All reconstituted solutions should be suitably protected from light also during administration (light-resistant infusion set).
Dosage :
The following regimes can be used :
Malignant Melanoma : Dacarbazine can be administered as single agent in doses of 200 to 250 mg/m² body surface area/day as an i.v. injection for 5 days every 3 weeks. As an alternative to an intravenous bolus injection dacarbazine can be administered as a short-term infusion (over 15 - 30 minutes). It is also possible to give 850 mg/m² body surface area on day 1 and then once every 3 weeks as intravenous infusion.
Hodgkin’s disease : Dacarbazine is administered in a daily dose of 375 mg/m² body surface area i.v. every 15 days in combination with doxorubicin, bleomycin and vinblastine (ABVD regimen).
Adult soft tissue sarcomas : For adult soft tissue sarcomas dacarbazine is given in daily doses of 250 mg/m2 body surface area i.v. (days 1 - 5) in combination with doxorubicin every 3 weeks (ADIC regimen). During dacarbazine treatment frequent monitoring of blood counts should be conducted as well as monitoring of hepatic and renal function. Since severe gastrointestinal reactions frequently occur, antiemetic and supportive measures are advisable. Because severe gastrointestinal and haematological disturbances can occur, an extremely careful benefit-risk analysis has to be made before every course of therapy with dacarbazine.
Duration of therapy :
The treating physician should individually decide about the duration of therapy taking into account the type and stage of the underlying disease, the combination therapy administered and the response to and adverse effects of dacarbazine. In advanced Hodgkin’s disease, a usual recommendation is to administer 6 cycles of ABVD combination therapy. In metastasized malignant melanoma and in advanced tissue sarcoma, the duration of treatment depends on the efficacy and tolerability in the individual patient.
Rate of administration :
Doses up to 200 mg/m2 may be given as a slow intravenous injection. Larger doses (ranging from 200 to 850 mg/m²) should be administered as an i.v. infusion over 15 - 30 minutes. It is recommended to test the patency of the vein first with a 5 to 10 ml flush of sodium chloride infusion solution or glucose 5 %. The same solutions should be used after infusion to flush any remaining drug from the tubing. After reconstitution with water for injections without further dilution with sodium chloride infusion solution or glucose 5 %, dacarbazine 100 mg and 200 mg preparations are hypo-osmolar (ca. 100 mOsmol/kg) and should therefore be given by slow intravenous injection e.g. over 1 minute rather than rapid intravenous bolus injection over a few seconds.
Special populations :
Patients with kidney/liver insufficiency :
If there is mild to moderate renal or hepatic insufficiency alone, a dose reduction is not usually required. In patients with combined renal and hepatic impairment elimination of dacarbazine is prolonged. However, no validated recommendations on dose reductions can be given currently.
Elderly patients :
As limited experience in elderly patients is available no special instructions for the use in elderly patients can be given.
Children :
No special recommendations for the use of dacarbazine in the paediatric age group can be given until further data become available.
CONTRAINDICATIONS :
DACONE is contraindicated in patients who have a history of hypersensitivity reactions to dacarbazine or to any of the excipients, in pregnant or breastfeeding women, in patients with leucopaenia and/or thrombocytopaenia, in patients with severe liver or kidney diseases,who have previously had severe myelosuppression.
WARNINGS :
Haematopoietic depression is the most serious form of toxicity and involves primarily the leucocytes and megakaryocytes causing depression of platelets, but also other blood forming elements. Leucopaenia and thrombocytopaenia may be severe enough to cause death. Careful monitoring of red and white blood cells and platelets is required. Haematotoxicity may warrant temporary suspension or termination of therapy. Hepatic toxicity accompanied by hepatic vein thrombosis and hepatocellular necrosis (Budd-Chiari Syndrome) resulting in death has been reported. The incidence of such reactions has been low, approximately 0.01 % of patients treated. This toxicity has been observed when dacarbazine has been administered concomitantly with other antineoplastic drugs; however, it has also been reported in some patients treated with dacarbazine alone.
PRECAUTIONS :
Toxicity : In the treatment of each patient, the physician must weigh carefully the possibility of achieving therapeutic benefit against the risk of toxicity. Administer only to patients in hospitals with an oncology service so that they can be observed carefully and frequently during and after therapy particularly for haematopoietic toxicity. Restriction of food intake for 4 to 6 hours prior to treatment may reduce the severity of nausea and vomiting which occurs in most patients particularly during the first 2 days of treatment. Administration of an antiemetic may also reduce the severity of these effects.
Impairment of liver and renal function : See Dosage and Administration
Avoid contact with the skin and eyes. Immunisation with live virus vaccines should only be undertaken with extreme caution. Immunisation with oral poliovirus vaccines should be postponed in people in close contact with the patient, especially family members. The bone marrow depressant effects of dacarbazine may result in an increased incidence of microbial infection, delayed healing and gingival bleeding. Dental work, whenever possible, should be completed prior to initiation of dacarbazine therapy, or deferred until blood counts have returned to normal. Patients should be instructed on proper oral hygiene during treatment, including caution in the use of toothbrushes, dental floss and toothpicks.
Pregnancy : Category C.
Dacarbazine has been shown to be mutagenic, teratogenic and carcinogenic in animals. It must be assumed that an increased risk for teratogenic effects exists in humans. Therefore dacarbazine must not be used during pregnancy.
Nursing mothers :
Although very little information is available regarding distribution of antineoplastic agents into breast milk, breast-feeding is not recommended while dacarbazine is being administered because of the risks to the infant. It is not known whether dacarbazine is distributed into breast milk.
Paediatric Use :
Appropriate studies on the relationship of age to the effects of dacarbazine have not been performed in the paediatric population.
Effects on ability to drive and use machines :
DACONE may influence the ability to drive or operate machines because of its central nervous side effects or because of nausea and vomiting.
INTERACTIONS AND INCOMPATIBILITIES :
Microsomal liver enzyme inducers :
eg. barbiturates, rifampicin, phenytoin may theoretically hasten the activation of dacarbazine to AIC.
Mercaptopurine, azathioprine, allopurinol :
Dacarbazine inhibits xanthine oxidase and may theoretically potentiate the activity of these drugs. The incidence or severity of side effects may be altered when dacarbazine is used in combination with other antineoplastic agents. The leucopaenic and/or thrombocytopaenic effects of dacarbazine may be increased with concurrent or recent therapy with other medications which cause these effects. Additive bone marrow depression may occur if dacarbazine is administered with other bone-marrow depressants or with radiation therapy. Dosage adjustment of dacarbazine may be necessary. Sequential administration of dacarbazine (400 - 1000 mg/m²) and fotemustine (100 mg/m²) has been associated with acute lung toxicity, in the form of adult respiratory distress syndrome. It has been reported that dacarbazine reduced the response to levodopa in a patient with Parkinson’s disease. The mechanism of this interaction is unclear, but since the plasma levels of levodopa were unchanged, it is unlikely to be due to pharmacokinetic changes.
Administration of dacarbazine may potentiate the replication of live virus vaccines, increase the adverse effects of the vaccine, or decrease the antibody response to the vaccine. Dacarbazine may also suppress the antibody response to killed virus vaccines. Viral vaccines should not be administered for 3 to 12 months after discontinuing immunosuppressive drug treatment.
SIDE EFFECTS :
More common reactions : Gastrointestinal : 90 % of patients experience nausea and vomiting in the first two days of treatment. Diarrhoea may also occur. A degree of tolerance may develop to these effects after about 2 days of treatment. Vomiting lasts 1 to 12 hours. Prophylactic antiemetic therapy with a 5HT3 blocker or dexamethasone is usually required. Rarely, intractable nausea and vomiting have necessitated discontinuance of dacarbazine therapy.
Haematological : bone marrow depression (25 %) (see Life threatening reactions). Leucocytopaenia was usually seen 14 days after commencement of therapy but was noted as early as day 10 and, in 10 % of patients, as late as day 30 (ie. 25 days after completion of therapy). The average length of duration was 1 week and the longest, 3 weeks. Thrombocytopaenia was most frequently seen 18 days after commencement of therapy but in 43 % of patients it was noted by day 12 and in 10 % not until after day 30. The average length of duration was 1 week and the longest 3 weeks. Eosinophilia has been reported in one patient receiving dacarbazine.
Less common reactions : Cardiovascular : facial flushing, ECG abnormalities, orthostatic hypotension. Hypotension appears to be associated with high doses (> 850 mg/m²) of dacarbazine and may be dose-limiting.
Dermatological : (1 %, usually transient) rash, alopecia. Photosensitivity reactions have occurred rarely.
General : (3 %) flu-like syndrome with fever to 39°C, severe myalgias and malaise. This syndrome usually occurs after large single doses approximately 7 days after treatment with dacarbazine and lasts 7 to 21 days. It may recur with successive treatments.
Hepatic : (5 %, usually transient). Increases in transaminases (AST and ALT), alkaline phosphatase, LDH. Levels usually return to normal within 2 weeks. Hepatic toxicity accompanied by hepatic vein thrombosis and hepatocellular necrosis (Budd-Chiari Syndrome) resulting in death has been reported (0.01 %). A case of acute hepatitis has been reported during the first course of dacarbazine. Granulomatous hepatitis has also occurred.
Nervous System : (3 % usually transient) blurred vision, seizures, headache, paraesthesia, confusion, malaise, lethargy.
Local reactions : Injection of concentrated dacarbazine solutions may cause severe pain along the vein. Extravasation of the drug into surrounding tissue may cause severe pain, tissue damage and cellulitis.
Hypersensitivity : Anaphylaxis has occurred occasionally.
Dental effects : Dacarbazine may adversely affect dental procedures.
Other : Dacarbazine may rarely cause stomatitis.
Life threatening reactions :
Bone marrow depression : Death due to agranulocytosis or thrombocytopaenia occurred in about 0.4 % of patients in clinical trials.
Fatal hepatotoxicity : Budd-Chiari Syndrome.
DACONE solution is chemically incompatible with heparin, hydrocortisone, L-cysteine and sodium hydrogen carbonate.

 Cardiovascular
Cardiovascular